Maintaining an adequate inventory of blood products to meet the needs of hospitals and patients is an essential role of blood banks. Blood stock levels are usually depleted within a few days and can vary widely depending on different factors such as the supply of different blood groups and donor availability.
Today’s global blood shortage has many reasons but if a patient is in a trauma situation blood is needed immediately, not in an hour or the next day. It is therefore crucial, that blood banks are not just responsible for collecting blood and finding blood donors, but that they also use blood products efficiently and handle blood resources with great care.
“Closing the blood product
supply chain cycle
is more important than ever.”
„
What is cold chain management?
„Storage conditions relate largely to the maintenance of temperature from the time of collection, through processing, testing and labelling and transportation, up to the point of issue for transfusion into a patient. This is known as „cold chain management“.1
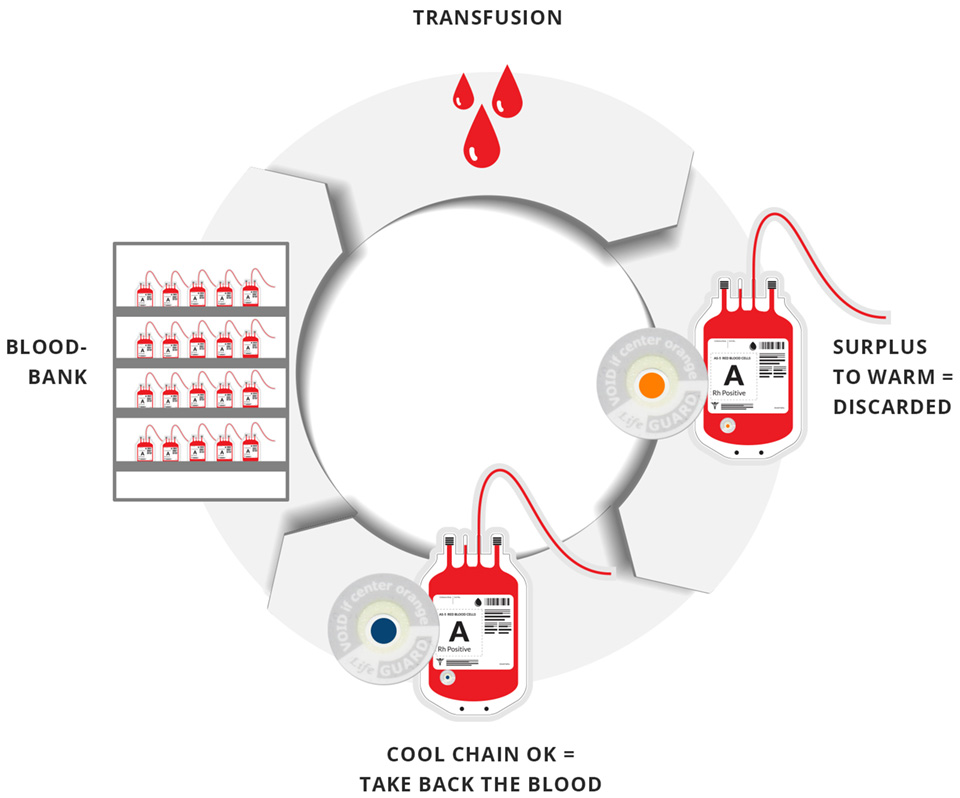
Sustainability and economic aspects demand that cold chain management should go one step further and ensure that unused blood products are returned to the blood bank safely. This is only permitted if the blood products have not exceeded critical temperature limits at any time – also during transport. Safely returning unused blood to storage requires that an efficient and permanent temperature monitoring system is in place.
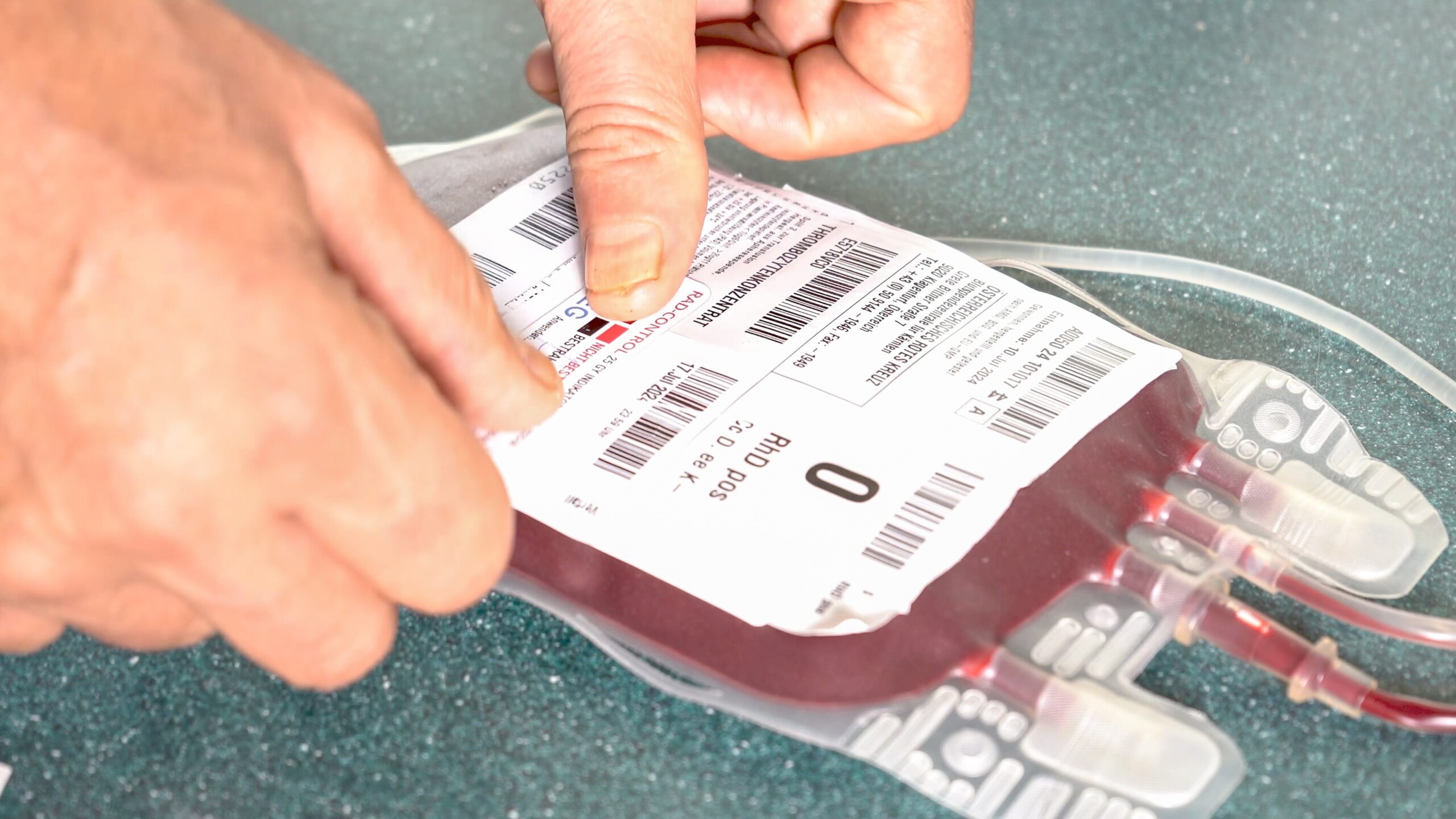
How are red blood cells (RBC) monitored during transport?
Strictest standards apply when it comes to storing blood products and monitoring their temperature during transport: temperature-controlled storage rooms, dedicated refrigerators designed to keep the blood and components within a specific temperature range and dedicated validated blood/component transport containers are used.
The list of temperature monitoring devices is also very long and ranges from conventional thermometers, chart recorders, electronic data loggers to computer-linked software.1 But the key question with all these solutions is: can these cold chain devices provide permanent and continuous temperature monitoring? Can we be sure that unused blood has not exceeded critical temperature limits at any time?
How does effective blood bag temperature monitoring work?
Life-Guard temperature indicators are specifically designed to close the cold chain cycle by permanently monitoring blood bag temperature. They can be applied on warm and cooled blood bags. Non-activated Life-Guard indicators are yellow.
A special UV-C light source ensures easy, quick and contactless activation of the indicators and turns them blue. Once activated, the indicators start monitoring the temperature. As soon as a critical temperature limit is exceeded, the indicators irreversibly turn orange. If the indicators stay blue, blood can be returned to storage and reused. Surplus blood products only need to be discarded if the indicators have changed in colour.
How sustainable is the cold chain cycle in the blood bank?
Closing the cycle of the cold chain blood bag supply makes it possible to use blood which is otherwise is discarded: only if the cold chain is fully intact and the blood temperature has never exceeded a critical level, blood bags can be returned if there is a surplus to requirements. However, the temperature must be constantly monitored to ensure the blood products and their recipients are safe.
Ongoing monitoring of blood temperature—from storage to distribution and back again—ensures that quality levels are not compromised. It guarantees that every blood donation is used carefully and not one needs to be discarded if not transfused. This is a solution every blood bank should seriously consider in times of severe blood shortages.
Sources:
1 ISBT Science Series (2020) 15, 232–254 © 2020 The Author. Journal Compilation © 2020 Blackwell Publishing Ltd. DOI: 10.1111/voxs.12599 ISBT Science Series, Section 12: Blood storage and transportation
picture credit: Shutterstock
Authors: Dr. Harald Sekljic, Dr. Clemens Troschl, Mag. Lisa Springer