Transfusion Medicine specialists have to check long protocols before making their clinical decisions and transfusing the right batch of blood. This process is not the place where you can make assumptions, interpretations or take any other forms of risk. For some patients it is vital that they receive irradiated blood to stop them from developing the almost always fatal Transfusion-associated Graft-versus-Host Disease (TA-GvHD). In this context, the key questions for each transfusion specialist are: Was the blood product I am using previously irradiated? Can we be sure? How can irradiated blood be differentiated from non-irradiated blood? What does the verification look like? Was the blood bag in question really inside the irradiator?
“The key question is:
was this particular blood bag
inside the irradiator?”
„
Why is blood irradiated?
The purpose of blood irradiation is to prevent the Transfusion-associated Graft-versus-Host Disease (TA-GvHD)—a possible complication of blood transfusion which occurs when viable donor T cells proliferate and engraft in immunodeficient patients after transfusion.”1 It is a delayed, serious and life-threatening reaction occurring later than 24 hours after the start of the transfusion. – Since the chances for successful treatment are minimal and TA-GvHD has a fatality rate greater than 90%, this transfusion reaction has to be prevented in the first place by exposing blood to irradiation.
“Irradiated blood is prepared by exposing the component to a radiation source (irradiator). The standard dose of gamma or X-ray irradiation in the US is 2500 centigray (cGy) targeted at the central portion of the container with a minimum dose of 1500 cGy delivered to any part of the component.”2 Verifying that irradiation was correctly performed is vital for patients who are at risk of developing this rare disease.
How can we know for sure?
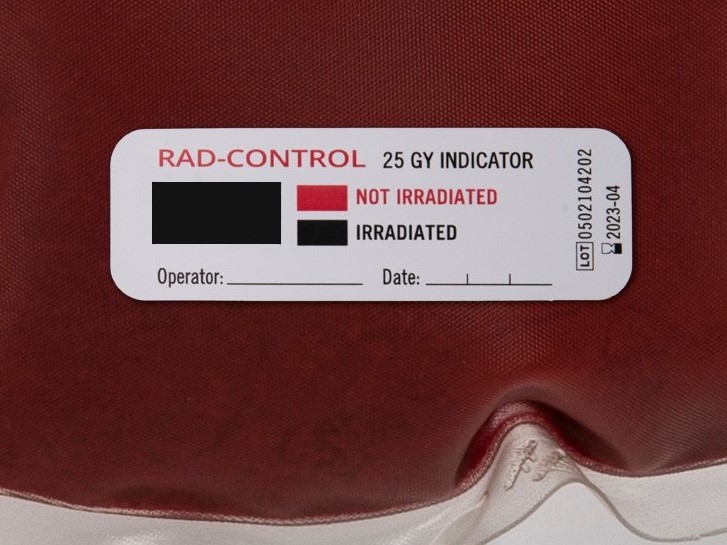
Blood irradiation indicators are the only verification tools to prove this process. These labels are affixed on each individual blood bag when preparing for irradiation. After the process, the indicator field on the labels has changed from red to black or alternatively has turned into an electronically readable irradiation result. Either way the different types provide proof that each particular blood bag was exposed to irradiation and was actually inside the irradiator.
When transfusion medicine specialists are ready to transfuse they don’t rely on assumptions. They differentiate non-irradiated from irradiated blood by checking the indicator on the particular blood bag: it clearly indicates that irradiation was performed and the result was added into the IT system.
Why is it so important to have one label on each bag?
Not all transfusion medicine centres verify irradiation properly. Both regular dosimetry checks of the machine and the use of irradiation indicators are very important and shall not be ignored or confused. Unfortunately, this is not standard practice across the globe. Some countries and blood centres have not yet implemented the specific protocols for one indicator per blood bag. Whilst dosimeters check the machines and their performance, only irradiation indicators give proof that the relevant blood product was definitely placed inside the irradiator. This is the reason why an indicator should be attached on each bag prior to irradiation.
Check the blood, not the machine!
Some machines print labels showing proof of irradiation which can be affixed on the relevant blood bags after irradiation. This leaves room for human error when labelling the blood products. And since the dosage applied may vary in different spots inside the canister, it shows no proof that the radiation was in fact correctly applied to each blood bag. Some blood centres also reduce their use of indicators by adding one to each irradiation container. In that case, the colour change clearly shows that the irradiator worked but it is not sufficiently clear that each bag was actually exposed to radiation. It is very important to understand that irradiation indicators are not to be used as dosimeters or to check the proper functioning of the irradiation device. Their plain and only purpose is to differentiate non-irradiated from irradiated blood.
Do not make assumptions, verify!
In order to avoid the risk of handling mistakes, the correct strategy is therefore to use one blood irradiation indicator per blood bag. The Council of Europe’s EDQM Guide (2020) to the preparation, use and quality assurance of blood components states that “Radiation indicators must be used as a tool for differentiating irradiated from non-irradiated blood and blood components.”3 – a clear recommendation for one label per blood bag. The Serious Hazards of Transfusion Report (SHOT) 20174 also underlines this very important detail when preparing blood bags for irradiation: “At each step in the transfusion process, do not assume that no errors have been made in previous steps; verify each step.” Blood irradiation indicators indicate the irradiation step is complete and if attached to the blood bag, no assumptions have to be made when starting the transfusion process. The ISBT5 also confirms this recommended protocol by stating: “Radiation sensitive labels are commercially available and if attached to a unit being irradiated will indicate, by change of colour, that the process has been successfully completed.”
One blood bag, one label!
To wrap it up, there are three important points to remember:
- It is vitally important to use one indicator per blood bag. This is the only proof that the specific blood product was actually inside the irradiator and was exposed to the irradiation.
- A blood irradiation indicator may never be used as a dosimeter. Its only purpose is to verify blood irradiation, not the functionality of the irradiator.
- The correct way of verifying blood irradiation is to not to only check the machine but the blood product itself by using one irradiation indicator label on each blood bag!
Sources:
1 Sezer Saglam (2011). Blood Irradiation, Modern Approaches To Quality Control, Dr. Ahmed Badr Eldin (Ed.), ISBN: 978-953-307-971-4, InTech, Available from: www.intechopen.com/books/modern-approaches-toquality-control/blood-irradiation
2 AABB Circular of Information for the use of human blood and blood components, 2021-12, pp. 70ff
3 EDQM Guide to the preparation, use and quality assurance of blood components (2020): © Council of Europe, 2020, ISBN 978-92-871-8644-7 , p 188, 4.4.1.2
4 PHB Bolton-Maggs (Ed) D Poles et al. on behalf of the Serious Hazards of Transfusion (SHOT) Steering Group. The 2017 Annual SHOT Report (2018).
5 ISBT Introduction to blood transfusion © 2020 Blackwell Publishing Ltd. ISBT Science Series (2020) 15, 207–231








![[:de]Blutbesstrahlung vor einer Transfusion verhindert TA-GvHD[:en]Blood irradiation prior to transfusion prevents TA-GvHD[:]](https://onpointmedicals.at/wp-content/uploads/2021/11/What-is-blood-irradiation-scaled.jpg)