Blood irradiation is performed prior to transfusion for one reason only: to prevent transfusion-associated graft-versus-host disease (TA-GvHD), a rare but serious complication of a transfusion where donor T cells in transfused blood components establish an immune response against recipient tissues. It is far better for this disease to be prevented by blood irradiation than for it to be diagnosed. “Because TA-GvHD caused by donor engraftment is fatal in most cases, irradiated blood products should be provided to patients at risk whenever time and resources allow.”1
“Irradiation of blood components is used almost exclusively to prevent graft-versus-host disease (TA-GvHD).”
2020
„
Where is blood irradiation performed?
Blood is irradiated in specially designed irradiators dedicated exclusively to this task and usually located in blood banks or hospital radiotherapy units. Protocols describe the procedure and standardise exposure times. The functionality of the irradiator is constantly monitored by a dosimetry protocol.
Two types of irradiators are used. They work with either gamma rays or X-rays. Both have the same ability to inactivate T cells in blood components at a given absorbed dose. However, in recent years, gamma blood irradiators have increasingly been replaced by stand-alone X-ray irradiators.
How does blood irradiation work?
Blood irradiation is a process where blood is exposed to a minimum of typically 25 Gy of radiation (Gray [Gy] is a unit of measurement for ionising radiation). Blood products are modified by it and radiation prevents lymphocytes from being able to reproduce whilst causing negligible damage to the blood cells.
“Ionising irradiation eliminates the functional and proliferative capacities of T cells, leaving other blood components, especially red blood cells, granulocytes and platelets, functional and viable. This is possible because T cells are more radiosensitive than other blood components.”2 “For immunosuppressed or immunocompetent patients potentially suffering from TA-GvHD after transfusion, it is vital that T cells are modified so that they cannot attack host tissues.”3
Blood products can be called “irradiated” in the US, once 25 Gy of irradiation is targeted at the centre, with the equipment calibrated to deliver no less than 15 Gy to any part of the canister. In Europe, a minimum of 25 Gy has to be applied to any part of the blood product in the irradiator. In order not to harm the other blood components, the maximum dose is generally defined as 50 Gy. All details on dosage can be found in Standards for Blood Banks and Transfusion Services, 32nd Edition by The American Association of Blood Banks (AABB) as well as in the Guidelines on the use of irradiated blood components issued by the British Society for Haematology in 2020.
Why confirm that irradiation was carried out?
Why is it important to have positive confirmation that the irradiation process has been completed? This is necessary to identify whether an operator failed to initiate the electronically controlled irradiation process and to rule out the possibility that the irradiation process was not performed because of instrument malfunction.
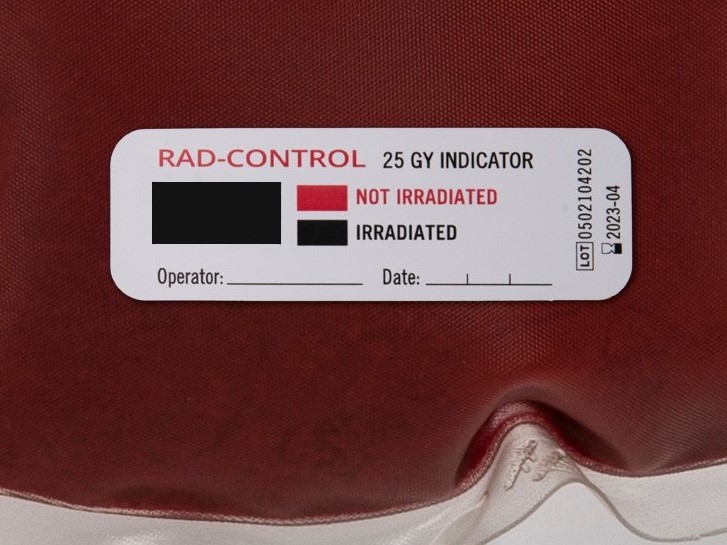
Radiation-sensitive indicator labels such as RAD-CONTROL® have been developed specifically for this purpose. The label is placed on the external surface of the blood product and irradiation causes distinct visually or electronically observable changes which verify that irradiation has occurred. The latest generation are barcode indicators which show an electronically readable result only after irradiation. This makes it possible to fully automate the documentation of the irradiation process.
It is important to understand though that the purpose of these indicator labels is merely to verify the irradiation process of blood products. They confirm that each individual blood bag was inside the irradiator and exposed to irradiation prior to transfusion. The labels are therefore no proof of any applied dosage and should never be considered a dosimeter.
For more on blood irradiation, listen to episode “Radioactive” of the Blood Bank Guy Essentials Podcast.
Sources:
1 Michelle L. Erickson, Chapter 6 – Indications for Transfusion and Dosing of Blood Components, Editor(s): Robert W. Maitta, Clinical Principles of Transfusion Medicine, Elsevier, 2018, Pages 53-67, ISBN 9780323544580, https://doi.org/10.1016/B978-0-323-54458-0.00006-4. (https://www.sciencedirect.com/science/article/pii/B9780323544580000064)
2 Sezer Sağlam, Demiroglu Bilim University , researchgate.net, 2011, Blood Irradiation*
3 Blood Bank Guy, Podcast episode 074CE, https://www.bbguy.org/
4 International Irradiation Association iia, White Paper: Uses and Applications of Radiation Processing, 2020, iiaglobal.com








![[:de]Blutbesstrahlung vor einer Transfusion verhindert TA-GvHD[:en]Blood irradiation prior to transfusion prevents TA-GvHD[:]](https://onpointmedicals.at/wp-content/uploads/2021/11/What-is-blood-irradiation-scaled.jpg)