Blood irradiation is performed prior to transfusion and for one reason only: to prevent transfusion-associated graft vs. host disease (TA-GvHD) occurring in immunosuppressed patients and neonates, a complication of transfusion that is almost always fatal. The irradiation process can presently be performed with either Gamma or X-ray irradiation.
“Either technology is suitable for
blood component irradiation.”
„
What is more effective?
A study presented at the 36th International ISBT (International Society of Blood Transfusion) congress compared X-ray and Gamma irradiation and the effects on the vitro quality of stored red cell and platelet components:
“There are a number of clinical indications where evidence supports the irradiation of blood components to inactivate cells to prevent transfusion-associated graft versus host disease. Gamma irradiators use a radioactive source, and are subject to rigorous health, safety, and compliance regulations due to the risks of nefarious or accidental dispersal. The effects of irradiation on red cell and platelet components are well known, however there is little or no data comparing the effects of X- and gamma irradiation on red cell and platelet component quality, or their ability to inactivate cells.The aim is to compare the in vitro quality of stored red cell components (standard, paediatric, washed and intra-uterine transfusion (IUT)) and platelet components (buffy-coat and apheresis) following X- or gamma irradiation, and to compare the ability of X- and gamma-irradiation to inactivate lymphocytes in blood components.”1
In summary and as a conclusion it was stated: „X- and gamma-irradiation have similar effects on the in vitro quality of stored blood components, and both effectively inactivate lymphocytes, indicating that either technology is suitable for blood component irradiation.“1 (Read the full conference paper)
Although both methods show similar outcomes, the worldwide trend has shifted from Gamma to X-ray. “There is international interest in moving away from using radioactive sources for gamma irradiation due to concerns with respect to biosecurity.“2 Therefore, gamma blood irradiators are increasingly being replaced by stand-alone X-ray irradiator machines worldwide.
Does a change of source affect the verification process?
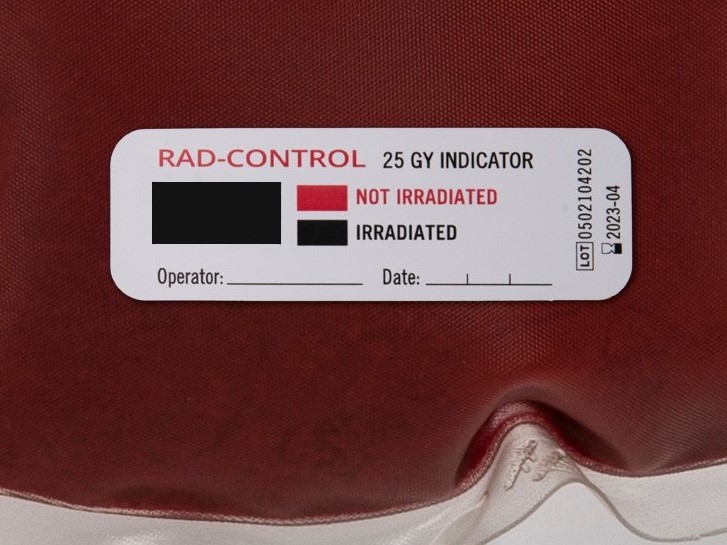
Radiation-sensitive indicator labels have been developed specifically to verify that irradiation was performed. These indicator labels ensure that each individual blood bag was inside the irradiator and exposed to irradiation prior to transfusion. Various brands offer either Gamma or X-ray irradiation indicators. A new source or change of irradiator always requires the validation of new indicators.
Rad-Control with all its variants is the only indicator label which can be used effectively and equally well for both Gamma and X-ray irradiation. Institutes planning to change their irradiator in the near future improve their workflow by using Rad-Control indicators suitable for both sources.
If you want to know more about the difference of Gamma and x-ray sources, read this comparison3.
Sources:
1 © 2020 The Authors Vox Sanguinis © 2020 International Society of Blood Transfusion Vox Sanguinis (2020) 115 (Suppl. S1), 1-1138 A comparison of x-ray and Gamma irradiation: effects on the in vitro quality of stored red cell and platelet components and efficacy of lymphocyte inactivation
2 Sezer Saglam (2011). Blood Irradiation, Modern Approaches To Quality Control, Dr. Ahmed Badr Eldin (Ed.), ISBN: 978-953-307-971-4, InTech, Available from: http://www.intechopen.com/books/modern-approaches-toquality-control/blood-irradiation
3 Radsource Technologies, Inc; www.radsource.com: Gamma vs X-ray Comparison








![[:de]Blutbesstrahlung vor einer Transfusion verhindert TA-GvHD[:en]Blood irradiation prior to transfusion prevents TA-GvHD[:]](https://onpointmedicals.at/wp-content/uploads/2021/11/What-is-blood-irradiation-scaled.jpg)